Great healthcare software doesn’t happen by accident. It’s built on thousands of invisible decisions: translations that never confuse, devices that never break the flow, tests that never sleep.
In the next few minutes, you’ll see how we helped Abbott scale all of this with full-cycle QA, and how localization, device coverage, and test automation became the foundation of a product trusted by millions.
What makes QA for healthcare SaaS uniquely difficult
This isn’t “high-stakes software.” It’s software where mistakes have names, dates, and consequences. Quality is the system that prevents them.
1. High-risk workflows with zero tolerance for error
Healthcare software testing must validate systems that influence diagnoses, treatment adherence, dosing, and clinical data interpretation.
FDA recalls show that 24–30% of medical software issues originate from incorrect data presentation or calculation errors.
Even minor UI faults, mislabeled units, truncated warnings, ambiguous instructions, can directly impact patient action.
Healthcare QA must validate not only functionality but clinical correctness, a dimension absent in typical SaaS.
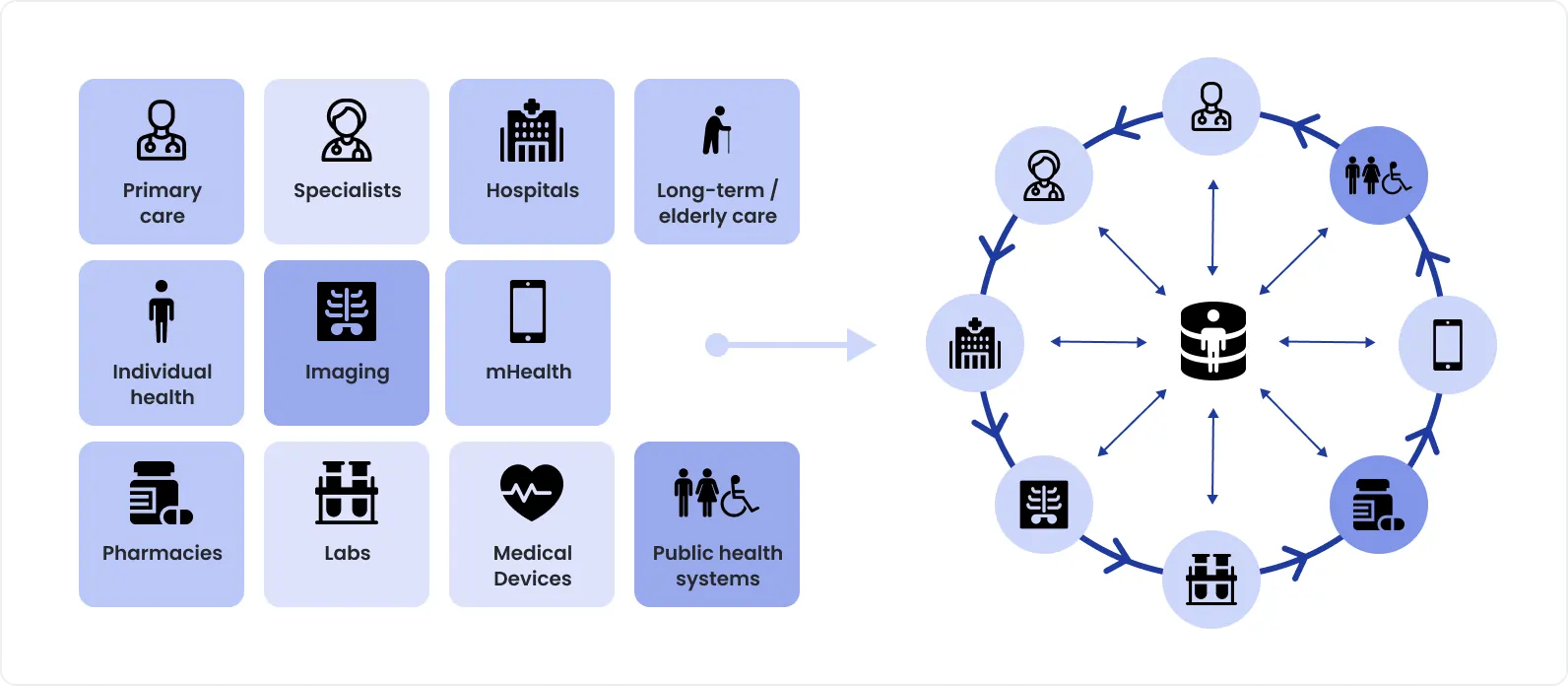
2. A fragmented, multi-platform ecosystem
Modern healthcare products require multi-device testing across web, iOS, Android, medical devices, wearables, and clinician dashboards.
The average mobile health app supports seven or more OS/version combinations at any given time.
Device fragmentation is increasing: Android alone has over 24,000 distinct device profiles in circulation.
QA must ensure continuity of data, consistency of workflows, and compatibility across an ever-expanding matrix, something manual testing simply cannot sustain.
3. Regulatory expectations: accuracy, reliability, traceability
Healthcare QA must produce evidence, not assumptions.
Regulations such as FDA 21 CFR Part 820, IEC 62304, and ISO 13485 require documented, repeatable, auditable testing.
Even minor failures can trigger mandatory CAPA processes, delayed releases, or fines.
This transforms QA from a “best practice” into a compliance-critical function.
4. Rapid release cycles under clinical and commercial pressure
Healthcare SaaS teams often ship updates weekly or bi-weekly to meet evolving clinical requirements, close security gaps, and stay competitive.
Across the industry, regression suites for healthcare apps average 3,000–10,000 scenarios.
Without test automation, regression cycles frequently stretch to 2–4 weeks, making modern CI/CD impossible.
Release velocity and safety must coexist, a balance enabled by QA automation for healthcare.
5. Global audiences with multilingual expectations
Digital health products increasingly serve worldwide patient populations.
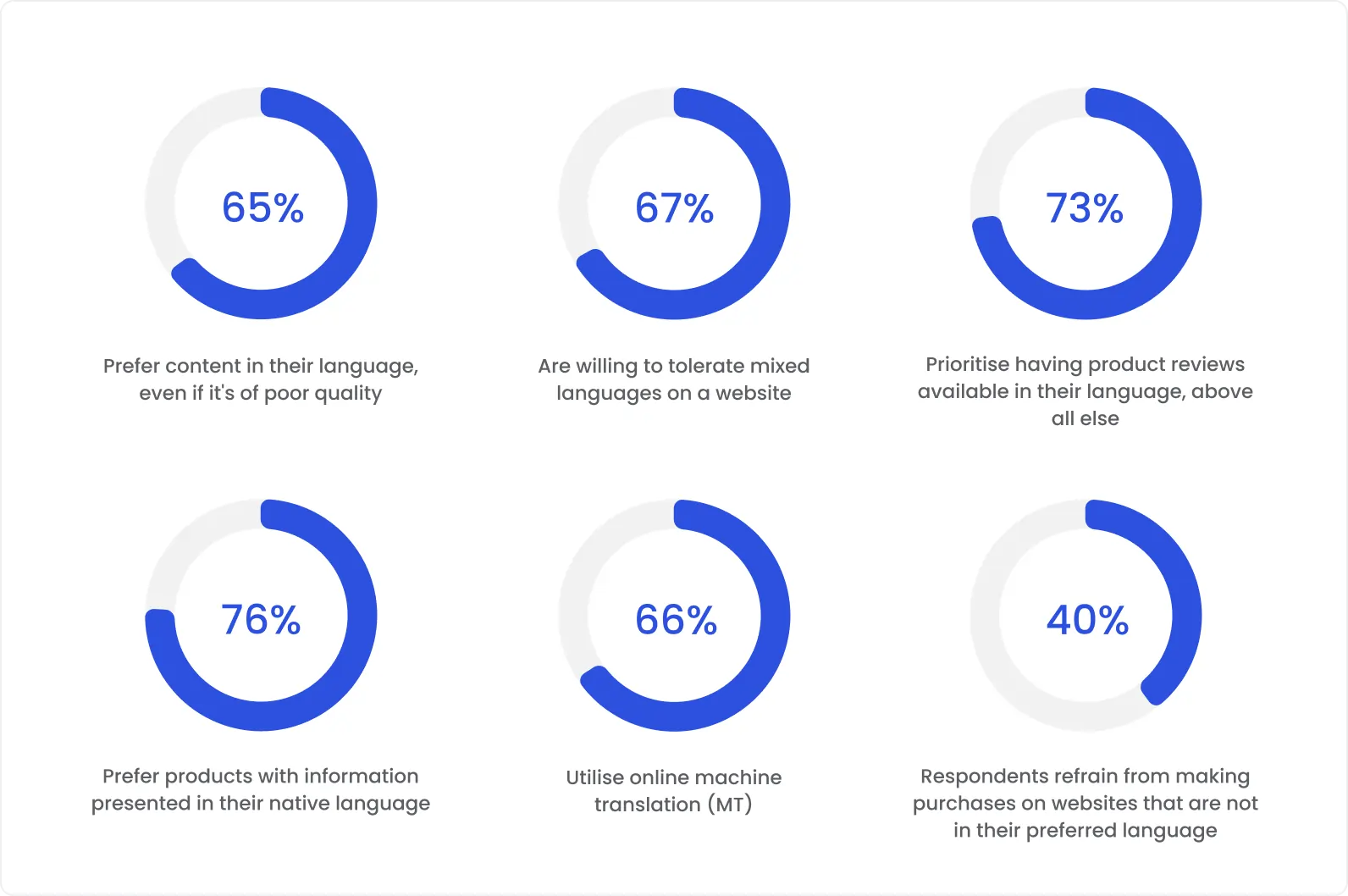
65% of global users prefer healthcare apps in their native language, and mistranslations remain one of the top causes of user abandonment in regulated markets.
Regulatory bodies in the EU, LATAM, and APAC now expect full language consistency, not partial coverage.
Localization defects in healthcare software testing are not cosmetic, they introduce clinical and compliance risk.
Why localization testing is a critical pillar of healthcare QA
In healthcare software, localization errors don’t show up as cosmetic issues, they surface as clinical risk.
Common, well-documented failure patterns include:
Incorrect units (mg/dL vs mmol/L) leading to misinterpretation of glucose levels. Even a simple unit mismatch can completely change how a patient or clinician reads the data.
Ambiguous warnings where severity is softened or unclear after translation, causing users to ignore critical alerts.
Truncated instructions in languages with longer words (German, Finnish), where UI layouts weren’t tested for expansion and vital information is cut off.
Date and number formatting errors (e.g., 03/07 interpreted as March 7 vs July 3), which directly affect logs, reports, and clinical timelines.
Industry incident analyses repeatedly show that language and presentation errors are a contributing factor in preventable clinical misunderstandings, especially in patient-facing digital tools. In healthcare, clarity is not a UX concern, it’s a safety requirement.
Managing 27+ localizations at scale: the Abbott LibreView case
LibreView, part of Abbott’s FreeStyle digital ecosystem, operates globally and supports patients, caregivers, and clinicians across dozens of countries. Localization at this scale can’t be handled manually or episodically.
In the Abbott LibreView engagement, DeviQA delivered healthcare localization testing across 27+ languages as part of a full-cycle QA strategy.
At scale, this required a structured approach:
Language packs validated not only for translation accuracy, but for formatting, units, and regulatory sensitivity.
Automated locale switching integrated into regression testing, so each build was verified across all supported markets, not just a subset.
Clinical terminology verification, ensuring that medical terms, labels, and report outputs remained correct and consistent across languages.
Consistent UX across markets, so workflows, charts, and warnings behaved identically regardless of language or region.
This eliminated a common healthcare risk: features that work correctly in one language but fail silently in another.
Why healthcare products can’t rely on partial language coverage
Partial localization is one of the most dangerous shortcuts in healthcare SaaS.
Real-world consequences include:
Users switching language mid-flow and encountering untranslated error states or warnings.
Critical help text or onboarding steps appearing in English while the rest of the product is localized.
Regulatory reviewers flagging incomplete language coverage as a compliance gap, delaying market entry.
From a safety perspective, partial coverage introduces inconsistent understanding of the same clinical feature, depending on language or region. From a business perspective, it increases support tickets, erodes trust, and exposes the product to regulatory risk.
Every user, regardless of language, must receive the same meaning, the same warnings, and the same clarity. That level of consistency only comes from treating localization testing as a first-class, continuously validated part of QA.
Localization in healthcare SaaS is not an enhancement. It is a core pillar of patient safety, compliance, and global reliability, and the Abbott LibreView case demonstrates what it takes to do it right at scale.
Multi-device and multi-browser testing
Healthcare software is used across fragmented, real-world scenarios, and the numbers reinforce how complex this is.
Over 70% of patients interact with digital health tools on at least two devices (mobile + desktop).
Clinicians commonly review the same patient data across 3–4 environments: clinic systems, web dashboards, tablets, and shared caregiver views.
Patients routinely move phone → laptop → clinic → caregiver account. The expectation is non-negotiable:
Data must be identical
Timelines must align
UX must stay stable
A missing data point or a chart behaving differently on another device instantly breaks trust, and in healthcare, broken trust equals perceived clinical risk.
Supporting 20+ device and browser combinations: the Abbott case
LibreView operates at global scale, which makes “test on the latest Chrome” meaningless.
As part of healthcare software testing services, DeviQA validated Abbott LibreView across 20+ real device and browser combinations.
Coverage included:
4 major browsers (Chrome, Safari, Firefox, Edge), each with different rendering engines.
Multiple OS versions across Windows, macOS, iOS, and Android, including older versions still widely used in clinics.
Mobile device fragmentation, especially on Android, where devices differ by manufacturer, screen size, and OS customization.
End-to-end integration flows:
medical device → mobile/web app → cloud → reports accessed by clinicians and caregivers.
This ensured not just UI consistency, but data integrity across the entire ecosystem, regardless of access point.
Avoiding silent failures that appear only on specific devices
The most dangerous defects in healthcare apps often affect a small percentage of users, and escape detection.
Industry data shows:
~30% of mobile bugs appear on only one OS or device configuration
Cross-browser rendering issues account for nearly 25% of production UI defects
Typical examples:
A glucose graph misrendering only on one browser due to SVG or canvas differences.
Background data sync failing on a specific mobile OS version, delaying readings.
Date, time, or timezone discrepancies appearing only on certain locales or devices.
Touch or scaling issues that hide critical UI elements on particular screen sizes.
These failures don’t crash the system, they silently distort or delay information. Multi-device and multi-browser testing is what exposes these edge cases before they reach patients and clinicians.
At global scale, consistency isn’t about polish. It’s about ensuring that every user sees the same data, every time, regardless of device, browser, or location.
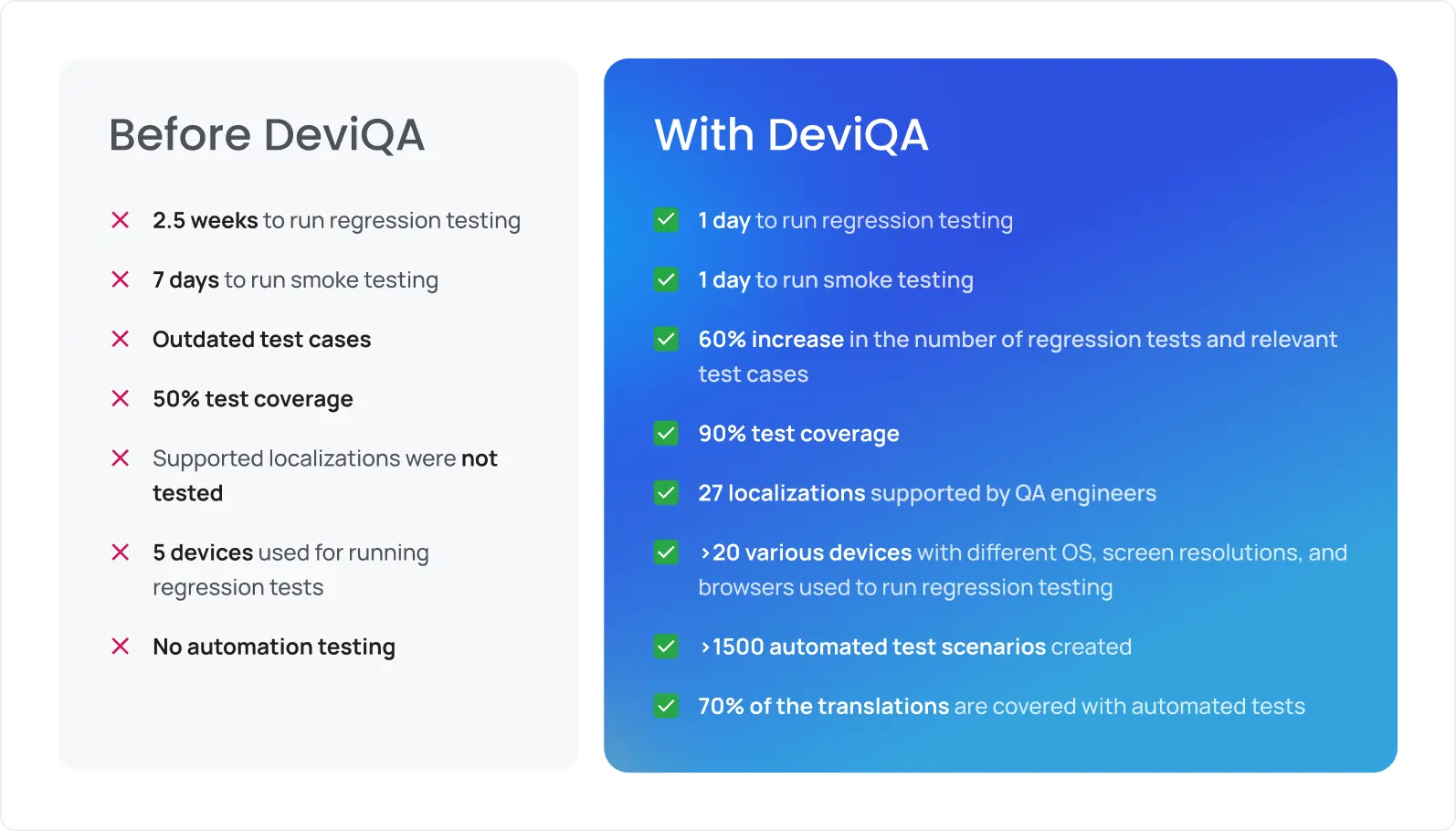
The test automation advantage
Healthcare software must move fast, without breaking trust — which is why QA automation for healthcare SaaS is essential.
Why manual-only QA collapses at scale
Healthcare applications accumulate complexity faster than most SaaS products, and regression grows with every release.
A mature healthcare platform typically includes:
Thousands of regression scenarios across clinical workflows
Multiple languages, devices, and integrations
Strict requirements for repeatability and traceability
Manually revalidating this surface area release after release turns QA into the bottleneck. In practice:
Regression cycles stretch into weeks
Releases get delayed or pushed with reduced coverage
Teams are forced to choose between speed and safety, an unacceptable tradeoff in healthcare
Manual QA can support early-stage products, but it cannot sustain regulated healthcare software testing at scale.
What test automation delivered for Abbott
The Abbott LibreView platform required frequent releases without compromising clinical reliability. Through QA automation for healthcare, Abbott transformed testing from an operational bottleneck into a predictable, scalable system.
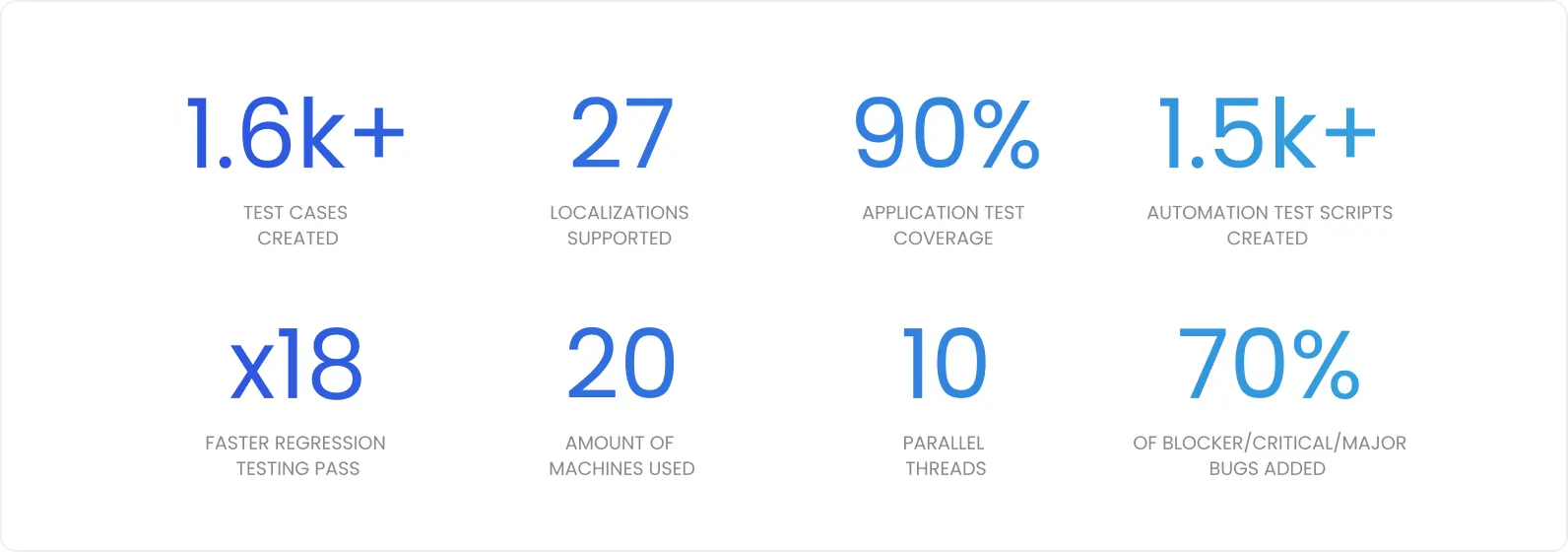
In the Abbott engagement, DeviQA delivered tangible outcomes:
Regression testing reduced from 2.5 weeks to 1 day
Smoke testing reduced from 7 days to 1 day
~90% automated test coverage
1,500+ automated test scenarios covering critical product flows
This shift allowed Abbott to release faster while increasing, not reducing, confidence in quality. Test automation didn’t just speed things up; it stabilized them.
Test automation across UI, API, and integration flows
Healthcare reliability depends on more than UI validation. Test automation must operate across the full system.
UI test automation verifies that patient-facing and clinician-facing workflows behave correctly across languages, devices, and browsers.
API-level test automation ensures data accuracy, validation rules, and error handling remain intact as backend services evolve.
Integration test automation validates end-to-end flows, from medical devices to mobile apps to cloud platforms and clinical reports.
Together, these layers prevent a common healthcare failure mode: components working in isolation while the full workflow silently breaks.
Full-cycle QA in practice: How all three areas work together
In isolation, localization testing, multi-device coverage, and test automation each solve part of the problem. In healthcare SaaS, that’s not enough. Reliability only emerges when all three operate as a single system.
Localization + test automation = scalable global releases.
For Abbott’s LibreView, supporting 27+ languages manually would have made every release slower and riskier. Test automation allowed localized builds to be validated continuously, ensuring that new features, fixes, and warnings stayed correct across every market without turning QA into a bottleneck.
Multi-device + test automation = consistent UX without manual overhead.
Automated regression across 20+ device and browser combinations ensured that charts, reports, and data flows behaved identically, regardless of how users accessed the platform. This removed the need for repeated manual validation while increasing confidence in every release.
Localization + multi-device = accurate experiences for every user segment.
Patients, caregivers, and clinicians interacted with LibreView across different devices, languages, and regions, yet saw the same data, workflows, and clinical meaning. Full-cycle QA made consistency the default, not something to be fixed post-release.
Together, this is what enabled continuous delivery without compromising safety. Abbott could release frequently, scale globally, and meet regulatory expectations, not because of one testing practice, but because quality was engineered end to end.
Conclusion
Healthcare SaaS teams don’t fail on quality because they don’t care. They fail because complexity outgrows informal processes. As products scale across users, regions, devices, and regulations, quality must be engineered, not hoped for.
Lessons every healthcare SaaS team should internalize:
Start test automation early, before regression becomes unmanageable
Treat localization as core functionality, not an afterthought
Test across real device and browser combinations, not ideal ones
Embed QA into CI/CD to prevent risk, not react to it
Validate clinical workflows end to end, not only the UI
Use dedicated QA teams to maintain ownership and continuity
Ensure data integrity across all environments
Healthcare has zero tolerance for inconsistency. A feature that behaves differently across languages or devices isn’t incomplete, it’s unsafe.
The Abbott LibreView case proves that full-cycle QA for healthcare SaaS enables fast, compliant, global delivery.
If you’re scaling a healthcare SaaS product and quality is becoming harder to control, DeviQA can help. With 15+ years of healthcare QA experience, we build full-cycle QA systems that protect patients, satisfy regulators, and support confident growth.
